Ending the Epidemic New York State Budget and Policy Priorities
State Fiscal Year 2022 – 2023
It is time for substantial reinvestment in the Plan to End New York’s HIV/AIDS epidemic.
We have made significant progress implementing the 2015 Ending the Epidemic (EtE) Blueprint recommendations developed collaboratively by HIV community members, providers, advocates, and New York State and local public health authorities. HIV surveillance data shows that, by the end of 2019, EtE efforts enabled us to “bend the curve” by decreasing HIV prevalence in NYS for the first time since the epidemic began, and to bring new HIV infections to an all-time low. However, the data also shows that while HIV health outcomes have improved across all communities, vexing and unacceptable disparities persist in HIV’s impact on Black, Indigenous and people of color (BIPOC), and that EtE progress in Upstate New York lags behind New York City. The COVID-19 pandemic has further exacerbated these inequities. While the HIV provider community has been agile and committed to mitigating the impact of the COVID crisis on our EtE efforts, barriers to HIV prevention and care posed by the pandemic suppressed HIV prevention, testing, and connection to care, and there has been a steep increase in premature mortality among people with HIV (PWH) due to heightened vulnerability to severe COVID-19 disease. The COVID-19 crisis has also brought tragic increases in substance use disorder and opioid overdose at a time when we are already falling short of EtE goals to improve drug user health and eliminate new HIV infections attributed to injection drug use, and thousands of New Yorkers with HIV continue to experience homelessness and housing instability in the face of a new and deadly risk of COVID infection.
Confronting these challenges to end the HIV epidemic for all New York communities requires bold new action to advance health equity, including structural changes in our HIV service delivery systems to address racism and implicit bias, meaningful investments on the social and structural determinants that we know drive HIV health inequities, and concrete efforts to improve drug user health, support sexual health and wellbeing, and end the co-occurring hepatitis C epidemic.
The End AIDS New York Community Coalition calls for the renewed commitment and substantial financial and political investments necessary to fully implement the EtE Blueprint and end AIDS as an epidemic in New York. To advance health equity and end AIDS for all communities, the End AIDS New York Community Coalition submits the following three-pronged policy agenda and related budgetary proposals:
- Declare Racism as a Public Health Crisis and Make Concrete Health System Investments to Promote Equity
- Recommit to ETE by Addressing Housing Access and other Key Social Determinants of Health
- Arrest the Worsening Injection Drug Use and Opioid Epidemics
Declare Racism a Public Health Crisis, Make Concrete Health System Investments to Promote Equity
Declare Racism a Public Health Crisis
Declare racism a public health crisis which is impeding Ending the Epidemic. A growing body of research demonstrates that centuries of racism in the United States has had a profound and negative impact on communities of color. The impact is pervasive and deeply embedded and this creates inequities in access to a range of social and economic benefits—such as housing, education, wealth, and employment. These social determinants of health are key drivers of health inequities within communities of color, placing those within these populations at greater risk for poor health outcomes. We urge Governor Hochul to declare racism a public health crisis during her State of the State address this January 2022 and subsequently direct specific actions by the New York State Department of Health (NYSDOH) and other State agencies to ensure a whole of government response to advance racial equity as a core principle and priority.
Invest in Structural Health Systems Changes
Continue to invest in HIV delivery systems changes that focus on structural competency, which examines larger social conditions, public policies and elements of our service delivery systems that give rise to unequal access and health equities. Investments need to be sustained to enable NYSDOH and the AIDS Institute to identify health equity metrics, collect social determinants of health data, train clinicians, etc.
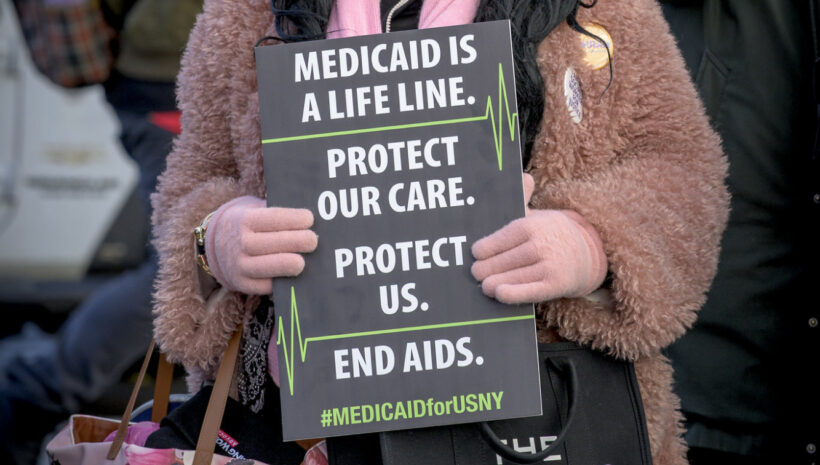
Protect the Healthcare Safety Net
Language in the FY22 New York State budget (HMH Article VII) delays the pharmacy benefit carve-out from Medicaid Managed Care to Fee-for-Service until April 1, 2023. We call on Governor Hochul to permanently repeal the Medicaid pharmacy benefit carve-out, as transitioning the pharmacy benefit to fee-for-service would eliminate the mechanism that enables safety net providers to access savings from the federal drug discount program known as 340B. HIV service providers and community health clinics rely on 340B savings to support otherwise unfunded or underfunded services that are essential for effective health care for the most vulnerable low-income New Yorkers. 340B resources are critical to achieving public health goals and are key to addressing health inequities based on race, poverty and marginalization. We can curb pharmacy costs by regulating pharmacy benefit managers and contract pharmacies, without threatening our hard-fought efforts to end the HIV epidemic and reduce health inequities.
Adopt and Implement the New York State Hepatitis C Elimination Plan
$10M
The EtE Community Coalition is extremely pleased that on November 17, 2021, Governor Hochul authorized the release of the New York State Hepatitis C Elimination Plan, a set of concrete recommendations developed with broad community and expert input under the direction of a Statewide HCV Elimination Task Force (HCV TF) led by the NYSDOH and a community co-chair. The 28 individuals appointed to serve on the HCV TF represent diverse backgrounds and expertise such as HCV prevention, clinical care and treatment, research and public health policy, as well as lived experience. Convened in 2018, the taskforce completed its work in June 2019 on a comprehensive set of draft recommendations to eliminate hepatitis C across NYS. However, the NYS HCV Elimination Plan recommendations were never released by the previous Governor, and no funding was provided to begin implementation. We call on Governor Hochul to formally adopt the NYS HCV Elimination Plan, direct the NYSDOH to begin implementation of the Plan recommendations, and provide funding to support this critical and lifesaving initiative.
Expand Hepatitis C Testing
Expanded hepatitis C testing must be an essential element of any effective NYS hepatitis C elimination strategy. To improve identification and treatment of New Yorkers with hepatitis C, amend the NYS hepatitis C testing law to: i) require the provision of a one-time hepatitis C test for every individual age 18 and older, and for individuals younger than 18 if there is evidence or indication of risk activity; ii) require a hepatitis C screening test for all pregnant persons during each pregnancy; iii) require that if a hepatitis C screening test is reactive, a hepatitis C RNA (diagnostic) test be performed to confirm diagnosis of current infection; and iv) make the law permanent with no sunset date.
Repeal the Medicaid Global Spending Cap
The Medicaid global cap was introduced in 2011 as a mechanism to limit growth in Medicaid spending and instill discipline in Medicaid budgeting. The cap was set at an arbitrary, fixed moment in time and not designed to keep pace with program growth. Medicaid is a critical safety net program and is a lifeline for PWH. It should be afforded the opportunity to grow in times of economic downturn or hardship, such as the COVID pandemic, to meet real need. Placing a cap of the Medicaid program disproportionately impacts people living with disabilities, under-resourced communities of color and safety net providers, like community health centers and HIV service programs that rely upon Medicaid as a significant coverage source for their patient base. It is time to repeal the Medicaid global cap.
Ensure Adequate and Timely Rates for HIV Special Needs Plans
New York’s Medicaid Managed Care HIV Special Needs Plans (HIV SNPs) are highly effective in addressing the needs of PWH and those at heightened risk of HIV infection, achieving high rates of viral load suppression and dramatically lowered inpatient and acute care costs. However, rate setting delays and inadequate rates threaten to undermine their effectiveness. HIV SNPs receive rates as late as 21 months after their effective date, and limits imposed by the global cap have reduced SNP rates at a time when membership has expanded to include people of trans experience and other medically vulnerable groups. HIV SNP rates that are late and inadequate negatively impact the SNPs, providers, and most importantly, SNP members, by limiting the available provider network which impedes access and quality of care. Timely and adequate HIV SNP rates are essential to EtE efforts and greater health equity.
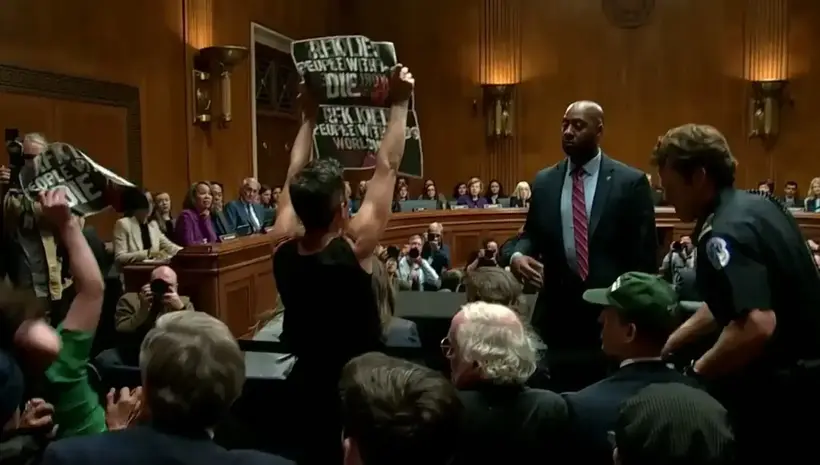
Exempt Lifesaving HIV Antiretroviral Drugs from Prior Authorization and Other Restrictions
Utilization tools such as prior authorization and step therapy can restrict access to medically necessary drugs. These barriers are harmful to patient access and can prevent individuals from receiving the medication they need in a timely manner. Delaying access to these medications for individuals who currently have, or are seeking to avoid, HIV/AIDS can be life threatening and stall the State’s EtE progress. Amend insurance law and § 272 of the Pub. Health Law to add new language that provides: “Antiretroviral drugs prescribed to a person enrolled in a public or private health plan for the treatment or prevention of the human immunodeficiency virus (HIV) or acquired immunodeficiency syndrome (AIDS) shall not be subject to a prior authorization requirement, step therapy, or any other protocol that could restrict or delay the dispensing of the drug.”
Address Severe Under-Investment in Infrastructure Needs of Nonprofit Organizations
Nonprofit human services organizations that have been on the front lines of both the HIV and COVID responses face ongoing and new challenges as the result of years of severe under-investment in essential infrastructure – leaving them struggling with inadequate or outdated systems for information technology, electronic data, financial management, human resources and other key functions. Building infrastructure capacity is not only essential to effective and efficient service delivery but will be required to in order for community-based nonprofit providers to prepare for, negotiate, and participate in coming value-based payment arrangements for service delivery. Inadequate State contract reimbursement rates not only limit the ability to invest in critical systems but leave nonprofit human services organizations at a serious disadvantage in an increasingly competitive labor market. Significantly, there has been no Cost of Living Adjustment (COLA) for human services providers in nine of the last eleven NYS budgets. It is time to invest in the infrastructure needs of nonprofits providing critical services for the most vulnerable New Yorkers. At a minimum, we urge the Governor to take action in this year’s budget to: i) increase the indirect rate on NYS contracts from the current 10% to a nonprofit’s established federally-approved indirect rate; and ii) provide a COLA increase of at least 5.4% in line with the July 2021 CPI.
Recommit to ETE by Addressing Housing Access and other Key Social Determinants of Health
It is well understood that the challenges posed by homelessness and housing instability, food insecurity, lack of employment, stigma, and other social and structural factors drive inequitable access to HIV testing, prevention, and care. Ample evidence also demonstrates that these factors are amenable to effective intervention that significantly improves HIV health outcomes. For that reason, the EtE Blueprint recommends concrete action to address social determinants of HIV health equity.
Provide Equal Access to Meaningful HIV Housing Supports Across New York State
$10M
Over 4,000 households living with HIV outside NYC remain homeless or unstably housed because EtE Blueprint recommendations to ensure access to safe housing as an evidence-based HIV health intervention have not been implemented Upstate or on Long Island. To provide Statewide access to meaningful HIV housing supports: i) amend the regulations governing the HIV Enhanced Shelter Allowance to set the rent payment standard for the program to at least 110% of HUD Fair Market Rates (FMR) for the locality and household size (the standard for Section 8 Housing Choice vouchers and other low-income rental assistance programs); ii) make the NYC-only HIV affordable housing protection available Statewide to cap the share of rent for low-income PWH at 30% of disability or other income; iii) require that each Local Department of Social Services (LDSS) provide all income-eligible PWH access to the HIV Enhanced Shelter Allowance and 30% rent cap upon request and application; and iv) notwithstanding other cost-sharing provisions, provide NYS funding to reimburse 100% of the cost of the HIV Enhanced Shelter Allowance and 30% rent cap in LDSS outside NYC.
Increase the Value of New York State FHEPS Vouchers
$TBD
Appropriate, affordable housing is also an effective HIV prevention strategy, providing the stability required to reduce exposure to HIV infection and to benefit from pre/post-exposure prophylaxis (PrEP/PEP). One potentially key program to address unmet housing need is the State Family Homelessness and Eviction Protection Supplement Program (State FHEPS), which creates a meaningful pathway for low-income families to enter safe and stable housing. However, at the current maximum rent level for the program of 85% of FMR, low-income families find themselves excluded from the housing market altogether, or forced into substandard, unsafe apartments. It is critical to increase the maximum rent level for State FHEPS vouchers to 110% of FMR, in line with Section 8 Housing Choice vouchers and other low-income rental assistance programs, to expand access to the appropriate housing opportunities desperately needed by families experiencing homelessness, particularly those who have experienced hardship or eviction due to the ongoing COVID-19 pandemic.
Expand Peer and Other Employment Opportunities
$4M
To increase opportunities for employment, vocational services, peer workforce placement, and economic mobility for PWH: i) increase OTDA funding to expand career readiness and job search assistance services and benefits counseling to PWH across NYS; and ii) establish a Peer Workforce Pilot Initiative through paid Peer Worker placements in health and social services organizations that will connect and maintain New Yorkers in medical care and housing. Peer workforce development investments address health disparities among PWH and achieve ETE goals by dramatically reducing new infections, increasing viral load suppression, and improving access to HIV treatment and care.
Expand Women-Focused HIV Services
$2M
Expand women-focused HIV testing, prevention, and early treatment access to reach women who test positive for sexually transmitted infections (STIs), survivors/victims of domestic violence, and women leaving correctional facilities, and establish a linkage and retention in care program for women with HIV outside of NYC.
Require LGBTQ+ Cultural Competency Training for All Licensed Providers
$1M
Amend Education Law §6507(3)(a) to allow the commissioner to establish standards requiring that all persons applying on or after April 1, 2022, to obtain or renew a license, certification, or registration for a limited permit to complete at a minimum two hours of coursework or training regarding LGBTQ+-related health care and overall LGBTQ+-related cultural competence. The following providers would be subject to these standards: physician, physician assistant, registered professional nurse, licensed practical nurse, chiropractor, dentist and dental hygienist, perfusionist, physical therapist and physical therapy assistant, professional midwife, podiatrist, optometrist, ophthalmic dispenser or optician, psychologist, social worker, massage therapist, occupational therapist, certified dietician, speech-language pathologist and audiologist, acupuncturist, athletic trainer, mental health practitioner, respiratory therapist and respiratory therapy technician or applied behavioral analysis.
Mandate HIV testing on an Opt-Out Basis in All Licensed Art. 28, 31, and 32 Facilities
$1M
Rates of concurrent HIV and AIDS diagnoses remain unacceptably high, especially among New Yorkers with limited access to primary care who may only interact with the health system in emergency departments or other institutional health settings. Amend the HIV testing law to facilitate true opt-out testing protocols with meaningful patient education and opportunity to decline testing, require that all licensed facilities employ opt-out HIV testing, and make technical assistance and/or consultation available from the AIDS Institute to assist with development of opt-out testing systems and protocols.
Expand NYS Sexual Health Clinics and Capacity to Provide PEP and PrEP
$10M
Sexually transmitted infections (STIs) continue to rise in NYS and nationwide, are too often undetected and untreated, and are linked to increased vulnerability to HIV. Expand STI, hepatitis C, and HIV testing and treatment and access to PrEP and PEP by increasing the number of Sexual Health Clinics in New York State and funding PEP and PrEP navigation at health care centers and community-based organizations, with a focus on increasing access to PEP and PrEP for African-American and Latina women, Asian and Pacific Islanders, and young adults, and through telehealth services to reach rural communities.
Broaden At-Home STI Testing
$1M
During the COVID-19 outbreaks of Spring 2020 in NYS, sexual health clinics across the state temporarily closed and significantly reduced hours which reduced access to STI testing. Meanwhile, STIs are projected to continue to increase. Although self-testing technology has advanced considerably there are barriers to its effective use. Direct NYSDOH to work with experts to identify current laws and regulations that pose barriers to home-based testing services (such as physical examination requirements), seek revisions to such laws and regulations to facilitate home testing, and establish and evaluate a pilot project of at-home STI screening.
Eliminate Congenital Syphilis in New York State by the End of 2030
$1M
Establish and implement a plan to eliminate congenital syphilis in NYS by the year 2030. Rates of syphilis in NYS continue to exceed the national average, ranking 11th in the nation in 2019. Left untreated syphilis can cause serious health problems such as tumors, blindness, nerve damage, and even death. However, if syphilis is identified quickly, it is curable with common antibiotics. Authorize NYSDOH to convene a statewide taskforce to develop comprehensive recommendations to improve screening, public and provider education, prevention and care.
Address HIV Health Disparities Experienced by Youth
Young New Yorkers, especially LGBTQ+ youth and young adults of color, continue to be disproportionately affected by HIV. Specific actions required to promote HIV health equity for youth and young adults include:
- Require Comprehensive Sexual Health Education: $22M Require all NYS public and charter schools to provide students in grades K-12 with integrated, comprehensive, developmentally appropriate, medically accurate and unbiased sexual health and HIV prevention education using a youth development approach, building on the strengths and capacities of young people.
- Implement a Condom Media Campaign: $2M Condoms are the only available primary prevention method against STIs for sexually active people. Condom usage in NYS declines every year, while STI rates increase.
- Increase Funding for LGBTQ Youth Services: $3M Increase grant funding available to providers serving LGBTQ youth.
- Develop and Deploy Novel Programs: $2M Novel strategies are needed to reach and engage young people in sexual health services. Youth rely on technology to meet their needs related to socialization, information, and even healthcare. Promising preliminary results from home HIV testing programs suggest that offering testing through mobile means is effective at reaching persons who otherwise cannot access testing through traditional channels. Telemedicine has the potential to make healthcare visits related to HIV and STI screening, as well as accessing PrEP/PEP, more convenient for persons who are unable to access these services because of transportation, stigma, fear, or other barriers.
Identify and Meet the Complex Needs of Older People with HIV
$2M
At the end of 2019, people aged 50 and older accounted for more than half of PWH living in NYS, underscoring the importance of identifying and addressing the more complex medical and social service needs of older PWH. Targeted strategies are required to provide access to comprehensive and integrated health care that is responsive to often-complex medical comorbidities, increase engagement of older PWH with behavioral health care, and develop programming to address social isolation, nutrition, exercise, mobility limitations, and other health maintenance needs.
Commit to Continue Core NYS EtE Funding Through at Least FY2025
$15M ($30M/2 years)
When year 2020 EtE goals were set in 2015, no one could have imagined the challenges presented by the COVID-19 pandemic or the impact of the COVID crisis on a range of related public health goals, from ending the HIV epidemic to addressing the opioid crisis. It is anticipated that year 2020 HIV surveillance data will show an artificially low number of new HIV diagnoses and a tragic increase in mortality due to severe COVID illness among PWH. Continuation of the $15 million ($30 million over two years) in Medicaid funding to support EtE strategies through at least fiscal year 2025 is essential to regain momentum and complete the work necessary to end AIDS as an epidemic and move closer to HIV health equity.
Arrest the Worsening Injection Drug Use and Opioid Overdose Epidemics
Scale-Up Harm Reduction Funding and Programming
$50M (Transfer from OASAS)
Harm Reduction programs provide essential, evidence-based services for people who use drugs including medical care, education, counseling, referrals, medication for opioid use disorder, and syringe exchange. Increase funding to improve drug user health, including syringe exchange programs, and peer support, which are in urgent need of reinvestment. Dedicate State funding for naloxone, a highly effective medication for reversing an opioid overdose. Establish and fund additional Drug User Health Hubs across the State, which offer a unique opportunity to provide on-demand care to people who use drugs, and Second-Tier Syringe Exchange Programs to serve hard to reach areas and individuals. Fund point of-care testing for HIV, STIs and HCV in Syringe Exchange Programs and Drug User Health Hubs, to substantially increase the capacity of the health system to screen for these infections in order to more rapidly engage people with use drugs in treatment and prevention. These critical efforts can be supported with an increased transfer of federal supplemental Substance Abuse Prevention and Treatment (SAPT) Block Grant program funding awarded to New York and other states to address the harmful effects of the COVID-19 pandemic for people with substance use disorder. The SAPT Block Grant is managed by OASAS in NYS, but the NYSDOH AIDS Institute is responsible for harm reduction programming and funding in the state. To date, OASAS has been awarded a total of $195.3 million in COVID-19 supplemental SAPT funds, of which we understand $52 million has been expended. The transfer of an additional $50 million in supplemental SAPT Block Grant COVID relief from OASAS to the AIDS Institute would provide the necessary resources to scale up highly effective harm reduction funding and programming across the state.
Approve and Fund Pilot Overdose Prevention Centers (OPCs)
$3M (Opioid Settlement Fund)
Approve, establish and evaluate five pilot Overdose Prevention Centers (OPCs) across the State to operate over at least two years. The pilot program will allow community-based organizations to operate OPCs, which offer sterile supplies and controlled settings for people to use pre-obtained drugs under the supervision of trained medical professionals who can intervene in case of an overdose. Support these efforts with funding from the Opioid Settlement Fund.